The Insulin System: Understanding How It Works
Insulin is a hormone at the center of how our bodies use food for energy. When everything is working properly, insulin helps keep our blood sugar (glucose) levels in a healthy range. However, problems can arise if our cells stop responding to insulin’s signals – a condition known as insulin resistance. The good news is that insulin resistance isn’t a permanent fate. By making some lifestyle changes in diet, exercise, stress management, and sleep habits, you can reduce or even reverse insulin resistance and improve your overall health. This article breaks down how the insulin system works in simple terms and offers practical, science-backed tips to enhance your insulin sensitivity for better wellness.
How the Insulin System Works
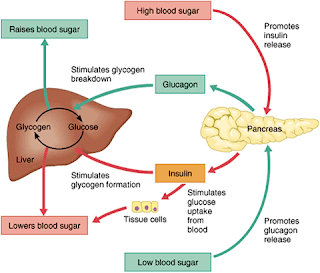
Insulin is often described as a “key” that unlocks our cells to let sugar in. After we eat, our digestive system breaks down carbohydrates into glucose (a type of sugar) that enters the bloodstream. In response, an organ called the pancreas releases insulin. Insulin acts like a key to let blood sugar into your body’s cells, which use the sugar for energy. As cells absorb sugar from the blood under insulin’s direction, blood sugar levels go back down to normal. This elegant system allows your body to fuel itself right after a meal and store any extra energy for later. For example, insulin signals the liver to store excess glucose for use between meals. In short, when insulin is working properly, it keeps blood sugar balanced: not too high after eating and not too low between meals. Most of the time, we don’t even notice this process – we eat, and our body handles the rest. However, issues with insulin can happen when the system is overworked or out of balance. To understand why insulin resistance is problematic, let’s first define what it means.
What Is Insulin Resistance?
Insulin resistance means your cells stop responding well to insulin’s “unlocking” signal. Even though insulin is present—often in higher-than-normal levels—the cells in your muscles, liver, and fat become less effective at absorbing glucose. Think of insulin as a key and your cell’s door as a lock that’s become rusty or jammed, making it hard for glucose to get inside where it’s needed.
This condition often develops when you consistently consume more sugar and refined carbohydrates than your body can use. High blood sugar forces your pancreas to produce extra insulin. Over time, your cells become desensitized to these high levels, and they no longer take in glucose as efficiently. At first, your pancreas may compensate by releasing even more insulin (a state called hyperinsulinemia), and you might not notice any symptoms. However, as insulin resistance worsens, the pancreas struggles to keep up, leading to elevated blood sugar levels, prediabetes, or even type 2 diabetes.
Insulin resistance also affects your body’s fat storage. When cells can’t absorb glucose properly, the excess sugar gets stored as fat, often around the belly. This can create a vicious cycle, as increased body fat can further worsen insulin resistance. Beyond blood sugar issues, insulin resistance is linked to other health concerns like high triglycerides, elevated blood pressure, and inflammation—components of what’s known as metabolic syndrome.
Because insulin resistance can develop without obvious symptoms, it often goes unnoticed until blood sugar levels are very high. The good news is that insulin resistance can be improved. With the right lifestyle changes, your cells can become more sensitive to insulin again, restoring the balance of your “key-and-lock” system.
What We Can Do
Eat a Balanced Diet to Support Insulin Function
Your food choices have a huge impact on how well your insulin works. An insulin-friendly diet focuses on whole, unprocessed foods that release sugar slowly and help keep your blood sugar steady. It’s not about “going hungry” – it’s about choosing the right balance of foods to fuel your body.
Here are some practical strategies:
- Pile on non-starchy vegetables: Fill half your plate with vegetables like broccoli, spinach, kale, peppers, cauliflower, and salad greens. They’re high in fiber, low in sugar, and help fill you up while keeping blood sugar levels steady.
- Choose high-fiber carbs over refined carbs: Swap refined grains (white bread, white rice, regular pasta) for whole grains such as whole-wheat bread, brown rice, oats, quinoa, or whole-grain pasta. Whole fruits are also a better choice than fruit juices or sweets.
- Cut back on added sugars and sweets: Foods and drinks high in added sugar—like sodas, candy, cookies, and cakes—can cause blood sugar spikes. Instead, save sugary treats for special occasions and opt for water, herbal tea, or sugar-free drinks in your daily routine.
- Include lean proteins with meals: Foods like fish, skinless poultry, beans, lentils, tofu, low-fat dairy, or lean meats help moderate blood sugar. Combining protein with carbohydrates slows digestion, so sugar enters your bloodstream more gradually.
- Favor healthy fats in moderation: Unsaturated fats from avocados, olive oil, nuts, and seeds can benefit insulin sensitivity. Use them in place of less healthy fats, but keep portions reasonable since fats are calorie-dense.
Also, how much you eat matters. Even healthy carbs in large portions can cause blood sugar surges. Pay attention to your hunger and fullness signals, and consider a gentle calorie deficit if weight loss is a goal. A balanced diet full of vegetables, fruits, whole grains, and lean protein can help keep your blood sugar steady, give your pancreas a break, and help your cells become more sensitive to insulin over time. Many people find these diet changes boost their energy and help shed excess weight, further improving insulin function.
Stay Physically Active to Boost Insulin Sensitivity
Exercise is one of the most effective ways to improve insulin sensitivity. When you’re active, your muscles absorb glucose from your bloodstream for energy, reducing the amount of insulin needed. Regular physical activity not only helps lower blood sugar but also reduces the risk of type 2 diabetes.
Here are some practical tips:
- Aim for consistent aerobic exercise: Try to get about 150 minutes of moderate-intensity activity per week—roughly 30 minutes a day, five days a week. Activities like brisk walking, cycling, or dancing can make a big difference. Even short sessions can boost insulin sensitivity.
- Include strength training: Building muscle through resistance exercises (like push-ups, squats, or light weightlifting) increases the number of cells that use glucose. Aim for strength workouts at least twice a week.
- Break up long periods of sitting: Even if you exercise regularly, make an effort to stand up and move around every hour. Short walking breaks or a few stretches can keep your metabolism active.
- Find activities you enjoy: You’re more likely to stick with exercise if it’s fun. Whether it’s hiking, dancing, or walking the dog, choose activities that make you smile.
Regular exercise not only helps your body use blood sugar more efficiently but also supports weight management—a key factor in improving insulin sensitivity. Even modest weight loss (around 5-10% of your body weight) can lead to significant improvements in blood sugar control. The best part is that making exercise a regular part of your routine benefits your metabolism regardless of weight loss.
Staying physically active is a powerful tool for enhancing your insulin sensitivity and overall health.
Manage Stress for Healthier Insulin Levels
Chronic stress can wreak havoc on your insulin system. When you’re stressed, your body releases “fight-or-flight” hormones like cortisol and adrenaline, which cause a spike in blood sugar to provide quick energy. This response is useful in short bursts, but constant stress—from work pressures, financial worries, or other challenges—keeps your body in high alert. Elevated cortisol makes it harder for insulin to remove glucose from your bloodstream, contributing to insulin resistance.
Reducing stress is a key part of improving insulin sensitivity. Lower stress not only helps balance your blood sugar but also prevents stress from triggering unhealthy habits like overeating or skipping exercise. Here are some strategies to tame stress and support your insulin health:
- Practice relaxation techniques: Deep breathing, meditation, progressive muscle relaxation, or gentle yoga can trigger your body’s relaxation response. Even a few minutes of slow, deep breathing can lower your heart rate and stress hormones.
- Stay socially connected: Sharing your feelings with a friend, family member, or counselor can be a great relief. Social support buffers stress—sometimes a simple walk or a good laugh with someone you care about is all you need.
- Make time for activities you enjoy: Engaging in hobbies like reading, cooking, gardening, or playing with a pet isn’t a luxury—it’s essential therapy for stress. Regular “me time” helps keep your stress levels in check.
- Get active: Exercise not only improves insulin sensitivity but also reduces stress by releasing endorphins and boosting mood. Even a brisk walk during a hectic day can help clear your mind and reduce stress.
By managing stress, you prevent these stress hormones from continuously interfering with your insulin function, helping your body maintain a healthier blood sugar balance. Think of stress management as another important tool—alongside diet and exercise—that moves you toward better overall metabolic health.
Prioritize Quality Sleep
Getting enough sleep is vital for insulin sensitivity. When you consistently skimp on sleep, your body becomes less efficient at using insulin—even if you maintain a healthy diet and exercise routine. Studies show that even a short period of sleep deprivation can make people more insulin resistant, while improving sleep can quickly boost insulin sensitivity.
During deep sleep, your body undergoes restorative processes that balance hormones. Without enough sleep, stress hormones like cortisol can rise, and other hormones that regulate appetite and growth may become disrupted. This imbalance can lead to higher blood sugar and increased insulin resistance.
The solution is simple: make sleep a priority. Most adults need around 7–9 hours per night for optimal functioning. To improve your sleep:
- Keep a consistent sleep schedule: Go to bed and wake up at the same times every day, including weekends.
- Create a relaxing bedtime routine: Wind down with activities like reading, a warm bath, light stretching, or deep breathing. Avoid screens and intense work before bed.
- Optimize your sleep environment: Ensure your bedroom is comfortable, dark, and cool. Consider blackout curtains or an eye mask and use earplugs or white noise if needed.
- Mind your caffeine and alcohol intake: Limit caffeine in the afternoon and evening, and consume alcohol in moderation, avoiding it close to bedtime.
- Watch your evening meals: Avoid large meals or heavy snacks right before bed to prevent discomfort and blood sugar spikes.
Improving your sleep habits can enhance your daytime energy, mood, and even reduce cravings. In short, getting enough quality sleep isn’t wasted time—it’s a key investment in a healthier metabolism.
Putting It All Together for Better Health
Insulin resistance can be a silent troublemaker, but it is largely reversible through lifestyle changes. By eating a nutritious diet, staying active, managing stress, and prioritizing sleep, you support your body’s natural insulin function. A balanced diet fuels your body, exercise helps your cells use that fuel efficiently, stress management keeps disruptive hormones like cortisol in check, and quality sleep helps restore insulin sensitivity.
Start small and stay consistent—you don’t have to change everything overnight. Try adding an extra serving of vegetables to your meals, taking a 20-minute walk each day, practicing a short breathing exercise in the morning, or setting an earlier bedtime. Over time, these small changes can boost your energy, focus, and mood as your body becomes more balanced.
It’s also a good idea to work with your healthcare provider, especially if you have prediabetes or other health concerns. They can monitor your progress and offer personalized guidance. While medications or supplements might sometimes be necessary, lifestyle modifications remain the first and most powerful step in reducing insulin resistance.
Improving insulin sensitivity isn’t just about preventing diabetes—it benefits your overall health, supporting your heart, brain, and joints. With every healthy meal, every walk or workout, and every stress-relief or sleep improvement, you help your cells work more efficiently. Treat insulin like your body’s fuel gatekeeper: nourish it well, move regularly, keep stress at bay, and rest enough. With patience and consistency, you can reduce insulin resistance and enjoy the benefits of a healthier metabolism. Here’s to a healthier life!
Updated 3/9/2025